Imagine a street. This street has a hundred residents all aged over 65. Now imagine the next street over. This street has a hundred residents aged 85 and over. How many of the residents of these two streets do you think are likely to be frail?
The British Geriatric Society estimates that one in 10 over 65s are likely to be affected by frailty increasing to up to one in every two for over 85s. That’s 10 residents of our first street and up to 50 in our second street, a total of 60 residents over just two streets!
You may say this is purely hypothetical, and, of course, you’re probably right. So instead imagine a county. That county had a total of 320,277 over 65s in 2023. Some 44,445 of these were aged 85 and over. Given what we know about frailty, that could represent 32,028 residents aged 65 and over who are impacted by frailty, with as many as 22,223 aged 85 and over. That county? That’s Essex today.
We can further develop our understanding. Using ONS population projections, we can estimate that by 2030 that frailty number will rise by nearly 5,000 among the over 65s across Essex. This is a huge increase in just six years’ time.
As AgeUK outlines, frailty describes an individual’s physical resilience and ability to overcome health issues quickly. That means that for frail individuals, health problems that might otherwise be thought minor, quickly become more serious. This is concerning for both the individual and the health and care system. Frail adults are known to be at higher risk of falls, attendance to hospital, and other long-term support. Our own analysis demonstrates that this has an impact on social care too, with adults who are more frail receiving services sooner than those that aren’t.
But, as NHS England tell us, we know that frailty is a largely preventable condition. Its onset can be limited through lifestyle improvements related to alcohol intake, maintaining physical activity, and a host of other factors. As a system, there is action we can take to prevent, reduce, and delay the onset and progression of frailty. The North East Essex Health Alliance is aiming to do exactly that. Previously, our team completed some work to support the roll-out of the Frailty Toolkit in that area. This toolkit encourages clinicians to refer patients who receive a Rockwood Clinical Frailty Score to specialist services that can help prevent their condition deteriorating using comprehensive and proactive assessments.
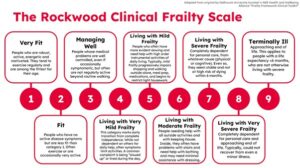
Now, we’ve gone one step further. Using linked health and care datasets we’ve built up a comprehensive view of patients' pathways through the health and care system. Specifically, we sought to understand what happened to patients within a 14-day window following the recording of a frailty score. Were patients referred on to services as set out in the frailty toolkit? For the most part no. We found that 78% of patients didn’t receive a referral to any service within that window, with referrals to dedicated frailty clinics exceptionally low.
Working with our stakeholders we identified several likely reasons for this ranging from simple things like the patient already being supported by a service, to data completeness issues such as referrals being made to internal primary care services and not being flagged in our datasets. We also found that the stakeholder considered ways of working to be a factor, with clinicians either unsure where to refer patients or lacking the time to do so.
But these are not insurmountable issues, and our insight has provided our stakeholders with evidence to continue encourage these referrals, through communications and discussions with clinicians. We’ve been able to argue the case for referrals following a frailty score by quantifying outcomes in the form of health and care service use. Findings suggest that service use are higher for frail patients compared to those who are non-frail, as well as those referred compared to those who aren’t.
As we continue to improve on these outcomes, we can encourage intervention to occur earlier in the frailty scale through the use of Proactive Care Assessments and Comprehensive Geriatric Assessments that have a track record of working for our patients. In future, we hope to return to the service to understand whether these proactive interventions are improving outcomes for patients.