Nerdy fact alert, but did you know that frailty is classified as a “syndrome” rather than a disease?
Diseases typically have a known cause, a distinct course, and an established pathway of care. In contrast, syndromes like frailty generally don’t have any of these ‘helpful’ features.
I think this technical distinction says so much about why frailty poses such a challenge to health and social care – impacting the services delivered by clinicians and carers in all settings, whether that be in a person’s home, at the GP, or in a hospital. As a result, making sure people are getting the right kind of care at the right time is vital.
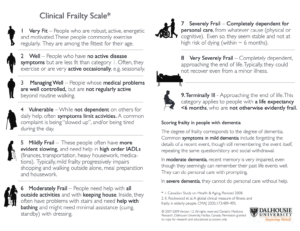
We’ve been supporting North East Essex Health alliance in its rollout of the Clinical Frailty Scale toolkit across general practices in North East Essex. The scale itself is a simple but clinically proven tool to categorise a patient’s level of frailty on a 9-point scale (as shown in the image below). In fact, anyone can do a clinical frailty scale assessment (with a bit of training) and the NHS has even made an app for it.
The toolkit the alliance has developed includes helpful prompts for clinicians depending on a patient’s score. These range from referrals to a GP care advisor, into a frailty clinic, or to strength and balancing classes – the latter being an intervention known to reduce adult social care need through a reduced risk of falling.
To support this effort, we were excited to use Suffolk and North East Essex ICB’s population health management data: a secure and pseudonymised patient-level record linking across the whole gambit of health and social care. Until very recently, such a valuable resource simply did not exist. This data makes it possible to deliver insight that captures the entire breadth of people’s health and social care journeys, helping Essex County Council to make holistic and proactive decisions.
Funnily enough, when I chat to friends about my work, they are surprised that different health and social care services weren’t already regularly sharing data.
The insight we delivered examined the current use of the Clinical Frailty Score. Giving just the headline findings, we found that:
- Clinical Frailty Scale assessments were typically targeted at patients with the highest levels of frailty. This was the case regardless of a patient’s age bracket, though because frailty generally increases with age, older patients are more likely to be scored. This raised questions for the alliance and its practices as to how proactive they wanted to be.
- Practices differed from one another both in the general levels of usage of the scale and the patients they targeted. Some practices bucked the overall trend, using the scale to assess patients with middling levels of frailty. This could be due to differences in patient population and the specific interests of practitioners based at the practices.
Last month we were invited to present our findings to the Clinical Directors across North East Essex. This garnered significant interest and a desire to share the findings more widely. The alliance is using our work to support a proactive care pilot that’s currently running and will use it to guide further phases and expansions. They are also using it to guide focus areas for practices across North East Essex.
There’s more to come for this project. The alliance’s Director of Operations has commissioned ECC Data and Analytics to examine the “so-what” question around the scale. We are embarking on a new programme of analysis all about assessing the effectiveness of the scale in kick-starting key referrals like strength and balance classes. We are hoping to deliver our first findings late September so watch this space!